The go to blog for ambitious professionals, who want to create sustainable career success despite chronic illness.
The 'Tired but Wired' Blog
Read this post →
You know that feeling when you’ve barely made it to 10am and already feel like you’ve run a marathon That used to be my norm, especially when I was pushing through chronic fatigue, trying to match the energy of colleagues who didn’t share the same health challenges. I thought a good morning routine meant 5am wake-ups, cold showers, and power yoga before sunrise. Spoiler alert: it didn’t work. What I needed was to build a morning routine for energy and focus.
And that’s what I want to help you do today.
Whether you’re dealing with fatigue, brain fog, or physical symptoms that make mornings unpredictable, you can still create a routine that supports you instead of draining you. Here’s how.
Why Morning Routines Matter (Especially When You’re Managing Chronic Illness)
Morning routines aren’t just trendy productivity hacks, they’re your foundation. The first hour of your day sets the tone for how you’ll think, feel, and function.
When you’re living with chronic illness, every decision costs energy. So, building a routine that helps conserve energy rather than waste it is key to a sustainable workday.
Here’s what a supportive morning routine can do:
- Stabilise your nervous system
- Prevent energy crashes later in the day
- Help you feel grounded, not overwhelmed
- Set realistic expectations for the rest of your day
Step 1: Let Go of “Perfect” and Start with “Possible”
If your current routine involves hitting snooze 5 times and stumbling into emails before coffee, don’t worry, you’re not alone. And you don’t have to overhaul your entire morning overnight.
Instead of aiming for an ideal morning, start with what’s doable.
Ask yourself:
- What 1 thing helps me feel more like myself in the morning?
- What’s draining me that I could remove or delay until later?
Maybe it’s replacing phone scrolling with 5 minutes of gentle stretching. Or swapping your morning coffee for a hydration boost (tip: caffeine can drain energy long-term, more on that in my free guide here).
Step 2: Anchor Your Routine with a Non-Negotiable
Pick one small thing that sets the tone for your day, no matter what else is going on. I call this a morning anchor.
Your anchor could be:
- A 3-minute breathing exercise
- A moment of quiet journaling
- Making your bed to signal “day mode” has begun
- Eating a low-sugar breakfast (great for stable energy!)
These small wins build momentum and give you back a sense of control, even when your body feels unpredictable.
(Need ideas? My free guide ‘5 Powerful Strategies to Reduce Fatigue at Work’ includes energising morning tips you can start tomorrow.)
Step 3: Prepare the Night Before
I know this is a post about mornings, but one of the biggest energy-saving moves happens before you sleep.
Try setting out your clothes, prepping a simple breakfast, or even just writing down 3 gentle goals for tomorrow. It gives your future self one less decision to make.
If you’re using tools like Notion or digital planners, take a look at this post from Marie Poulin for workflow ideas that support your routine.
Step 4: Adjust for “Flare-Up Friendly” Mornings
Some days, you’ll wake up with fewer spoons than usual. On those days, your routine still matters, but it should flex with your energy.
Here’s how:
- Swap your full routine for a “low energy version” (e.g. sitting stretches instead of a walk)
- Give yourself permission to delay anything non-essential
- Practice nostril breathing or a grounding technique from your bed
Remember: consistency doesn’t mean perfection. It means coming back to your anchors when you can.
Step 5: Make It Yours, Not the Internet’s
Forget what works for influencers or that productivity guru on LinkedIn. Your morning routine should reflect your life, your body, and your values.
If your energy is best first thing, build in focused work time. If mornings are your slowest, use them for rest, hydration, and movement, and schedule meetings later in the day.
This is your permission slip to design a life that fits you, not the other way around.
Want Weekly Support?
If you’re nodding along and thinking, “This is what I need more of,” then you’ll love my weekly newsletter: The Sunday Power-Up.
It’s a gentle boost in your inbox every Sunday with tools, tips, and stories to help you build a life and business that works with your energy, not against it.
👉 Sign up here.
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.

Read this post →
You’re halfway through your workday, and suddenly, you hit a wall. Your body feels sluggish, your mind is foggy and no matter how much you push, you can’t seem to focus. Sound familiar? These hidden energy leaks in your work routine could be the culprit.
The good news? You don’t need to overhaul your entire workday to fix them. Small, intentional shifts can protect your energy, boost your productivity and leave you with enough stamina for the things you love outside of work.
1. Multitasking: The Productivity Myth
Multitasking might feel efficient, but in reality, it forces your brain to rapidly switch between tasks, consuming more energy than you realise. Research shows that switching tasks can reduce productivity by up to 40% and significantly increase mental fatigue. In fact, studies have found that multitasking can even lower your IQ. Forbes highlights how multitasking erodes productivity and cognitive function.
What to do instead: Try ‘time-blocking’ – dedicating set periods to specific tasks without interruption. Use the Pomodoro technique (25-minute focus sessions followed by 5-minute breaks) to keep your mind fresh while maintaining deep focus.
2. Always Being ‘On’
Notifications, emails and endless pings create a constant state of alertness, depleting your mental energy reserves before you even realise it. This heightened state of vigilance leaves you exhausted, making it harder to focus on meaningful tasks.
What to do instead: Set clear boundaries with notifications. Schedule specific times to check emails and messages rather than responding instantly. Consider using ‘Do Not Disturb’ mode, ‘Focus Mode’ or apps that limit digital distractions.
3. Poor Posture and Workspace Setup
An uncomfortable workspace doesn’t just lead to physical discomfort, it also drains your energy. Slouching, poor lighting and incorrect desk height force your body to work harder to maintain focus, increasing fatigue over time.
What to do instead: Optimise your workspace for ergonomic comfort. Ensure your screen is at eye level, your chair supports your lower back and your feet are flat on the floor. Small changes like using a wrist rest, adjusting screen brightness, or standing up every hour can prevent unnecessary energy depletion.
4. Skipping Breaks (or Taking the Wrong Kind)
Many professionals believe pushing through fatigue will help them get more done. In reality, skipping breaks leads to diminishing returns, making it harder to concentrate and increasing overall exhaustion.
What to do instead: Incorporate active rest – short movement-based breaks like stretching, deep breathing, or stepping outside. These breaks refresh both body and mind, helping you sustain your energy levels throughout the day.
5. Ignoring Hydration and Nutrition
Dehydration and unbalanced meals play a massive role in fatigue. Relying on caffeine or skipping meals can cause blood sugar crashes, leaving you feeling sluggish and unfocused.
What to do instead: Start your day with a protein-rich, low-sugar breakfast to maintain steady energy levels. Keep a water bottle nearby and set reminders to drink throughout the day. Reducing caffeine after midday can also prevent energy crashes later in the afternoon.
Take Control of Your Energy
Small changes can lead to big results. By identifying and addressing these hidden energy leaks, you’ll be able to work efficiently without draining yourself. The goal isn’t to work harder, it’s to work smarter, so you still have energy left for life outside of work.
For more strategies to protect your energy at work, download my free guide: 5 Powerful Strategies to Reduce Fatigue at Work. It’s packed with practical tips to help you stay productive without burning out.
Looking for ongoing support? Subscribe to my newsletter, The Sunday Power-Up, for expert insights, real-world strategies and exclusive resources straight to your inbox. Let’s redefine success without sacrificing your health.
What’s one work habit you’re ready to change? Let me know in the comments!
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.

Read this post →
What Is the Burnout Cycle?
The burnout cycle is a repeated pattern of overworking until exhaustion, recovering just enough to push hard again and then repeating the process. It often begins with the pressure to prove oneself, taking on too much and ignoring the early signs of fatigue. Over time, this leads to diminishing productivity, chronic exhaustion and a sense of failure when energy levels inevitably crash.
Burnout isn’t just about feeling tired, it’s a serious condition that affects both mental and physical well-being. According to Mental Health UK, burnout can cause long-term stress, reduced performance and even physical health issues such as chronic illness if not addressed. Recognising the signs early and taking steps to break the cycle is essential for long-term success and well-being.
Breaking this cycle requires not only better time management but also a mindset shift, acknowledging that sustainable success comes from balance, not relentless effort.
Breaking Free from the Burnout Cycle
If you’ve ever found yourself caught in a relentless pattern of pushing too hard, crashing and then doing it all over again, you’re not alone. For professionals managing chronic illness, this burnout cycle can feel impossible to break. But here’s the truth: sustainable success isn’t about grinding through exhaustion, it’s about working in a way that supports your health and energy.
Let’s explore five common mistakes that may be keeping you stuck, along with actionable strategies to shift towards a more balanced, fulfilling work life.
1. Measuring Success by Hours Worked
Many of us have internalised the belief that more hours = more productivity. But the reality? Working long hours often leads to diminishing returns, increased fatigue and lower-quality output.
What to do instead:
- Focus on outcomes, not hours. Define what ‘success’ looks like based on results, not the number of hours spent at your desk.
- Try energy-based time management. Prioritise your highest-energy periods for deep work and allow for intentional rest breaks.
2. Ignoring the Early Signs of Fatigue
Waiting until you’re completely drained before resting is like waiting for your car to break down before refuelling, it’s ineffective and costly. Fatigue isn’t something to push through; it’s a signal that something needs adjusting.
What to do instead:
- Learn your early warning signs of burnout (brain fog, irritability, body aches) and take proactive breaks.
- Implement micro-rests: short, intentional breaks throughout the day to recharge before hitting exhaustion.
- Grab your free guide, 5 Powerful Strategies to Reduce Fatigue at Work, for actionable ways to maintain energy levels.
3. Overcommitting (and Underestimating Recovery Time)
It’s easy to say yes to everything, especially when you feel pressure to prove yourself. But overloading your plate leads to stress, resentment and ultimately, burnout.
What to do instead:
- Before agreeing to a new task or project, ask yourself: Do I have the energy and capacity for this?
- Create ‘buffer time’ in your schedule. Don’t pack tasks back-to-back without space to reset.
- Practise saying ‘no’ or offering alternative timelines that align with your energy levels.
4. Feeling Guilty About Rest
Rest is not a reward, it’s a necessity. Yet many professionals feel guilt when they step away from work, fearing they’ll fall behind.
What to do instead:
- Reframe rest as a productivity tool: downtime fuels your best work.
- Schedule rest with the same importance as work tasks.
- Engage in ‘active rest’ – activities like gentle stretching, deep breathing, or short walks that restore energy without complete inactivity.
5. Relying on Willpower Instead of Systems
Relying on sheer willpower to get through the day is a losing strategy. Without systems in place, it’s easy to fall back into unsustainable work habits.
What to do instead:
- Automate and streamline tasks where possible as this reduces decision fatigue and conserves energy.
- Use tools like Notion, Trello, or Asana to prioritise tasks and track progress without overwhelm.
- Consider external support, whether that’s a Virtual Assistant, accountability partner, or structured coaching.
Next Steps: Create a Work Routine That Works for You
Breaking free from the overwork-recovery cycle isn’t about doing less, it’s about doing what matters in a way that’s sustainable. By recognising these common mistakes and making small, intentional shifts, you can reclaim your energy and create a fulfilling work-life balance.
📩 Want more strategies like this delivered straight to your inbox? Subscribe to The Sunday Power-Up for weekly insights on balancing ambition with well-being.
💡 Ready to reduce fatigue at work? Download your free guide, 5 Powerful Strategies to Reduce Fatigue at Work, and start implementing energy-saving techniques today!
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.

Read this post →
You push through, day after day, trying to keep up with your workload. But no matter how much effort you put in, you end each day feeling depleted, foggy-headed and like there’s nothing left for your personal life. If this sounds familiar, your work might be draining your energy in ways you haven’t realised.
For professionals managing chronic illness, traditional career advice often falls short. ‘Work harder’ isn’t an option when energy is a limited resource. The key is recognising when your job is working against you and making changes before it takes a serious toll on your health.
Here are three critical signs that your work is draining you and what to do about it.
1. You’re Always Recovering from Work, but Never Feeling Rested

The Sign: You finish work and immediately need to crash. Whether it’s lying in bed for hours, zoning out on social media, or skipping activities you used to enjoy, your post-work life revolves around recovery.
Why This Happens: When your job requires more energy than you have, your body shifts into survival mode. Over time, this leads to burnout, chronic fatigue and even physical symptoms like headaches or muscle pain.
What to Do Instead:
- Assess your energy drainers. Keep a simple log for a week to track which tasks leave you most exhausted.
- Incorporate active rest. Instead of collapsing after work, try restorative activities like gentle stretching, breathwork, or even a short walk outside.
- Reduce energy leaks. Identify unnecessary tasks, meetings, or responsibilities you can delegate, automate, or remove entirely.
Want more strategies to prevent work-related fatigue? Download my free guide: 5 Powerful Strategies to Reduce Fatigue at Work.
2. Your Productivity Swings Between Overdrive and Shutdown
The Sign: Some days, you’re hyper-focused, racing to get everything done before your energy crashes. Other days, even the smallest task feels overwhelming and you struggle to get started at all.
Why This Happens: This boom-and-bust cycle is common for those with limited energy reserves. On high-energy days, you push through everything, depleting yourself. On low-energy days, your body forces you into shutdown mode.
What to Do Instead:
- Pace your workload. Instead of cramming everything into one high-energy day, break tasks into smaller, manageable chunks.
- Schedule strategic rest. Plan recovery breaks before you need them, not after you’ve crashed.
- Use energy-matching. Align tasks with your natural energy levels, save deep-focus work for peak times and reserve admin tasks for lower-energy periods.
This approach isn’t about doing less; it’s about working smarter. For weekly tips on sustainable success, join my newsletter.
3. You Feel Like You’re Losing Yourself to Work

The Sign: Work dominates your thoughts, even outside of working hours. You no longer make time for hobbies, relationships, or the things that bring you joy. Your identity feels tied to productivity and slowing down makes you feel guilty.
Why This Happens: When work consumes too much of your physical and mental energy, other parts of your life shrink. Over time, this leads to resentment, disconnection and the feeling that you’re losing yourself.
What to Do Instead:
- Reconnect with what matters. What did you love doing before work took over? Set small, manageable goals to reintroduce those activities.
- Redefine productivity. Success isn’t about doing more; it’s about creating a work-life balance that aligns with your values.
- Set boundaries and stick to them. Block off non-negotiable time for yourself, even 10 minutes a day can make a difference.
If work is draining you to the point of exhaustion, it’s time to rethink your approach. Small, intentional changes can help you reclaim your energy and create a career that supports your well-being instead of depleting it.
Know Your Rights: Flexible Working in the UK
If your job is affecting your health, exploring flexible working options could be a game-changer. In the UK, employees have the right to request flexible working arrangements, including remote work, adjusted hours, or job sharing. Employers must consider these requests in a fair and reasonable manner.
Understanding your rights can help you create a work schedule that better aligns with your energy levels and well-being.
For more information, visit GOV.UK – Flexible Working and Your Rights.
Next Steps: Protect Your Energy Before It’s Too Late
Waiting until burnout hits isn’t an option. By recognising these signs early, you can take control and create a sustainable work-life balance and prevent work draining your energy.
Ready to take the first step? Download 5 Powerful Strategies to Reduce Fatigue at Work for immediate, actionable steps to protect your energy, without sacrificing your ambition.
For weekly strategies to help you work smarter (not harder), subscribe to my newsletter.
You don’t have to accept exhaustion as the price of success. You deserve a career that works for you, not against you.
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.
Read this post →
Have you ever felt completely drained at the end of a workday, even when you love what you do?
If your career doesn’t align with your values, energy levels, or personal needs, it could be taking a greater toll on your well-being than you realise.
Many professionals push through fatigue, thinking burnout is just part of success. But when your work constantly depletes you, it’s a sign that something needs to shift. Realigning your career to match your energy and personal goals isn’t just about job satisfaction, it’s about protecting your long-term health and quality of life.
In this post, we’ll explore how career alignment influences your well-being, how misalignment manifests in stress and fatigue and practical ways to adjust your work so you can thrive.
How Misaligned Work Contributes to Fatigue and Stress
A career that doesn’t fit your personal values, energy levels, or well-being needs can impact you in several ways. Read on to find out how…
1. Energy Depletion from Constant Overexertion
If your work requires more energy than you can sustainably give, it leads to chronic exhaustion. High-pressure roles, rigid schedules and unsupportive environments can make even simple tasks feel overwhelming.
What to do instead: Assess your workload and energy patterns. Identify tasks that drain you most and explore ways to delegate, automate, or modify them. Prioritise work that aligns with your strengths and natural energy flow.
2. Emotional and Mental Stress from Lack of Fulfillment
Work that lacks meaning or personal connection can leave you feeling unmotivated, leading to stress and burnout. If your daily tasks don’t align with your values, you may struggle with low engagement and constant mental fatigue.
What to do instead: Reflect on what truly matters to you in your career. If your current job feels misaligned, explore ways to integrate more meaningful work, whether through role adjustments, side projects, or gradual career shifts.
3. Physical Symptoms from Chronic Stress
Unaligned work doesn’t just affect your mood, it can manifest in physical symptoms like headaches, muscle tension and increased fatigue. Stress hormones spike when your nervous system is constantly on high alert, making it harder for your body to recover.
What to do instead: Incorporate micro-rests into your workday, like breathwork, short breaks, or standing stretches. If stress is persistent, consider whether a career shift or boundary-setting is needed.
The Connection Between Meaningful Work and Better Energy Levels
When your work aligns with your values, strengths and health needs, it feels energising rather than depleting. Here’s why:
- Intrinsic Motivation Boosts Productivity: When you’re engaged in meaningful work, it requires less mental effort to stay focused and productive.
- Less Decision Fatigue: Career alignment reduces unnecessary stressors, allowing your brain to focus on creative and strategic thinking.
- Increased Emotional Resilience: Feeling connected to your work builds a stronger sense of purpose, making challenges feel more manageable.
Making small, intentional shifts toward career alignment doesn’t mean quitting your job overnight, it’s about adjusting how and where you work so your career supports your well-being rather than working against it.
Want to find out more about what makes work meaningful? Check out this article from Harvard Business Review.
How to Identify Career Shifts That Support Both Ambition and Health
If you’re experiencing misalignment, here are a few steps to begin shifting your career toward a more sustainable path:
- Assess Your Current Work vs. Your Core Values
Ask yourself: Does my work reflect what truly matters to me? Identify any gaps between your personal values and your current role. - Track Your Energy Patterns
Keep a journal for a week to note which tasks drain vs. energise you. This helps pinpoint necessary adjustments, such as shifting tasks, adjusting schedules, or seeking a new work environment. - Explore Alternative Work Models
If traditional 9–5 work isn’t sustainable, consider flexible work options like remote work, freelancing, or part-time roles that fit your energy needs. - Communicate Boundaries Clearly
Set realistic expectations with colleagues and employers. Advocate for accommodations that support your health while maintaining productivity. - Seek Support and Resources
Career shifts are easier with guidance. Consider professional coaching or communities that focus on sustainable career success.
Aligning Your Work for Long-Term Well-Being
Career alignment isn’t about working less, it’s about working in a way that supports your ambitions without depleting your energy. By making mindful shifts, you can create a career that fuels your well-being rather than draining it.
Ready to take the next step? Download my free guide, 5 Powerful Strategies to Reduce Fatigue at Work, for immediate steps to protect your energy and work smarter.
And if you want ongoing strategies to sustain your work-life balance, join my weekly newsletter for practical tips and insights!
Finally, if you’re looking for deeper guidance on aligning your career with your well-being, check out my coaching services to get personalised support on your journey.
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.
Read this post →
Do you ever feel completely drained at the end of the workday, like you’ve given everything you have and there’s nothing left?
When you’re managing chronic illness, fatigue isn’t just “feeling a bit tired”, it can be all-consuming, affecting both your work and personal life. But what if I told you that some of your daily work habits might be making your fatigue worse?
The good news? Small changes can make a huge difference. Let’s break down five common energy-draining habits and explore smarter ways to manage your day that will reduce fatigue at work.
1. Pushing Through Fatigue Instead of Taking Breaks
Why It Drains Your Energy:
Many professionals believe that “powering through” is the key to productivity. But ignoring your body’s signals leads to energy crashes, making it harder to recover and sustain performance throughout the day.
What to Do Instead:
✅ Use strategic rest – Try the 90-minute work cycle: work for 90 minutes, then take a 10–15-minute break.
✅ Incorporate micro-breaks – Stand up, stretch, or do deep breathing for 1–2 minutes every 30–45 minutes.
✅ Embrace active rest – Switch tasks instead of staying locked in one type of work for hours.
➡️ Want more powerful ways to manage fatigue at work? Download my free guide: 5 Powerful Strategies to Reduce Fatigue at Work.
2. Constant Multitasking and Context Switching

Why It Drains Your Energy:
Your brain isn’t designed to juggle multiple high-focus tasks at once. Constantly switching between emails, meetings, and deep-focus work increases cognitive load, leading to mental fatigue and decreased efficiency.
What to Do Instead:
✅ Batch similar tasks – Group emails, admin work and deep-focus tasks separately.
✅ Use the ‘single-tab’ rule – Keep only the essential windows open to avoid distraction.
✅ Set ‘Do Not Disturb’ time blocks – Protect deep work sessions to get more done with less effort.
➡️ Looking for sustainable work habits that boost energy? Join my weekly newsletter, The Sunday Power-Up, for practical tips.
3. Relying on Caffeine and Carbohydrates for Energy

Why It Drains Your Energy:
Caffeine and carbohydrates (particularly in the form of sugars) might feel like quick fixes, but they trigger energy crashes a few hours later, leaving you more exhausted than before. They also impact hydration and stress levels, making fatigue harder to manage.
What to Do Instead:
✅ Fuel your body properly – Start your day with a savoury breakfast instead of sugary cereals.
✅ Hydrate with intention – Replace some caffeine with electrolyte-infused water or herbal tea.
✅ Try a ‘caffeine cut-off’ time – Reduce afternoon caffeine intake to improve sleep quality.
4. Overloading Your Schedule Without Recovery Time
Why It Drains Your Energy:
If your calendar is packed back-to-back, you’re operating in survival mode, with no room for recovery. This can lead to burnout, brain fog and increased symptom flares if you’re managing a chronic illness.
What to Do Instead:
✅ Set realistic daily limits – Prioritise 3–5 essential tasks instead of overwhelming to-do lists.
✅ Schedule buffer time – Leave 15-minute gaps between meetings to reset your energy.
✅ Use the ‘No’ strategy – Protect your time by declining tasks that don’t align with your priorities.
➡️ Need help managing your energy at work? Download my free guide: 5 Powerful Strategies to Reduce Fatigue at Work.
5. Ignoring Your Body’s Signals

Why It Drains Your Energy:
Your body constantly gives you feedback, but in a culture that values productivity over well-being, it’s easy to ignore the signs. The result? You push too hard, triggering symptom flare-ups or complete energy crashes.
What to Do Instead:
✅ Use a symptom tracker – Record daily patterns to catch warning signs early.
✅ Redefine success – Shift from “doing it all” to doing what matters most for your well-being.
✅ Listen to your body’s rhythms – Identify when you have the most energy and schedule demanding tasks accordingly.
Final Thoughts
If you’ve been stuck in a cycle of overwork and exhaustion, you’re not alone. It’s time to break free from habits that drain your energy and replace them with sustainable work strategies that support both your ambition and well-being.
🔹 Want a deeper dive into practical ways to manage your energy at work? Download my free guide: 5 Powerful Strategies to Reduce Fatigue at Work.
🔹 Get weekly tips on balancing ambition with well-being by subscribing to The Sunday Power-Up newsletter.
🔹 The NHS provides expert-backed self-help tips for fighting fatigue, including practical advice on how to boost energy levels naturally. If you’re looking for additional ways to support your well-being, check out their full guide here: Self-help tips to fight fatigue – NHS.
💬 Which of these work habits do you struggle with the most? Let’s chat in the comments!
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.

Read this post →
January often begins with high hopes and resolutions, but it’s not uncommon for motivation to take a nosedive as the month goes on. For those of us managing chronic illness or burnout, the drop in energy can feel even more pronounced, making it difficult to keep up with the goals we set out to achieve. But that doesn’t mean all is lost. By embracing flexible goal-setting and celebrating small victories, you can keep moving forward in a way that honours your health and well-being.
Understanding the January Motivation Dip
It’s perfectly normal to experience a drop in motivation as January progresses. The initial excitement of a fresh start fades and reality sets in; especially when dealing with unpredictable symptoms and fluctuating energy levels. This can leave you feeling discouraged, but it’s important to remember that your worth isn’t tied to how much you accomplish. Your health and well-being should always come first.
Reframing Motivation with Chronic Illness
Instead of focusing on rigid goals that may not accommodate your health needs, try reframing how you approach motivation. Setting flexible intentions can help you adapt to your body’s demands without feeling like you’re failing.
Examples of Gentle, Adaptable Goals:
- “I’ll spend 10 minutes doing something that brings me joy, whether that’s reading, crafting, or enjoying a cup of tea.”
- “I’ll take one small step toward a project, like organising a single drawer instead of the entire room.”
- “I’ll prioritise rest and listen to my body, adjusting my plans if I need to.”
By allowing room for adjustments, you’re giving yourself the space to succeed on your own terms.
Practical Tips to Spark Motivation
Here are some simple ways to reignite your motivation while being gentle with yourself:
- Create a Vision Board: Use images, words and quotes that inspire you. Even on tough days, looking at your vision board can remind you of what brings you hope and joy.
- Schedule Micro-Adventures: Plan small, manageable activities that excite you, like a short walk in nature, trying a new recipe, or spending time with a friend. These mini adventures can lift your spirits and give you something to look forward to.
- Embrace Self-Care Rituals: Introducing new self-care practices, such as a warm bath with essential oils or a calming meditation, can be a way to nurture yourself and rekindle motivation.
The Power of Celebrating Small Wins
When living with chronic illness or managing burnout, progress often looks different. While society tends to celebrate big achievements, it’s crucial to acknowledge the small wins that are meaningful to you. Whether it’s getting out of bed on a particularly rough day, completing a simple task, or advocating for yourself at work, every effort counts.
Why Small Wins Matter:
- Boosts Confidence: Recognising your achievements, no matter how small, reinforces the belief that you are capable.
- Builds Momentum: Celebrating small successes can create a snowball effect, making it easier to tackle other tasks.
- Promotes Positivity: Focusing on what you have accomplished rather than what you haven’t can improve your overall outlook.
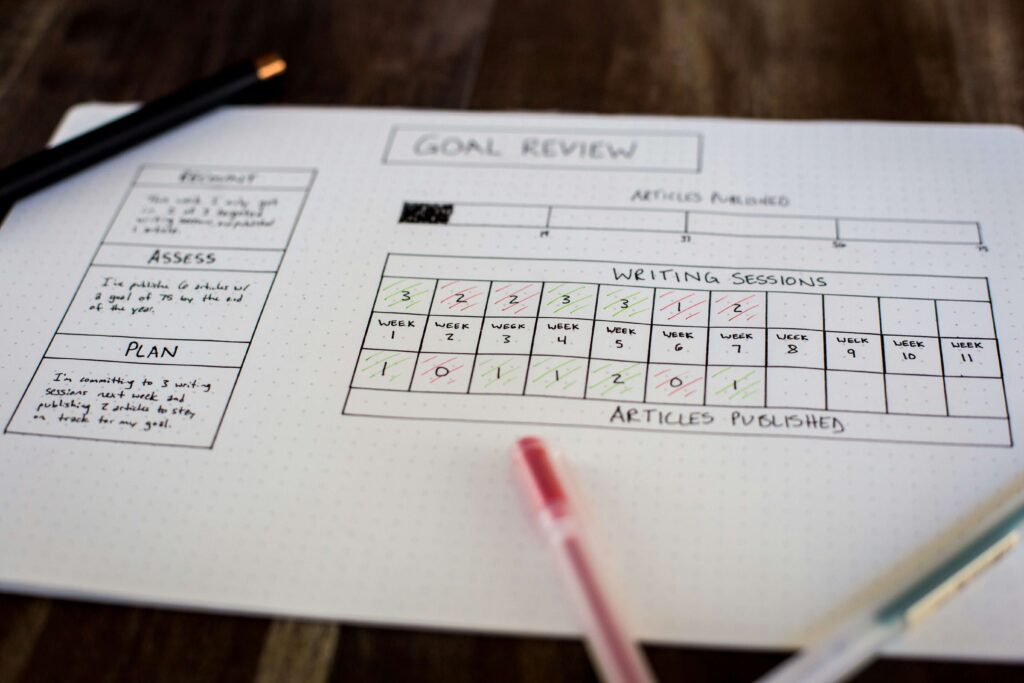
Tracking Your Progress
Keeping track of your progress can be both motivating and reassuring. Here are a few ways to do it:
- Journaling: Write down your wins each day, even if it’s something as simple as drinking enough water or resting when needed.
- Symptom-Tracking Apps: Use apps like Bearable to monitor how you’re feeling. Seeing your ups and downs over time can help you better understand your patterns and acknowledge the strides you’ve made.
- Gratitude Lists: End your day by listing a few things you’re grateful for, whether it’s the support of a loved one or a moment of calm in your day.
Final Thoughts
Navigating the new year with chronic illness or burnout is about finding your rhythm and honouring your unique journey. By setting gentle intentions, sparking motivation with small acts of joy and celebrating every win, you can create a year that feels balanced and fulfilling. Remember, it’s not about how fast you go, it’s about moving forward in a way that works for you.
If you’d like more insights and resources on managing chronic illness or burnout, sign up for my newsletter for weekly tips and encouragement. And for daily inspiration, follow me on Instagram @theemaspry.
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.

Read this post →
Navigating life with a chronic illness is already complex, but for those who are also neurodivergent, the challenges can multiply. Neurodivergence refers to variations in the human brain and cognition, which can include conditions like ADHD, autism, dyslexia, dyspraxia and more. Living with both neurodivergence and a chronic illness can create a unique and often overlooked set of experiences that impact daily functioning, well-being and the ability to thrive in a world that often isn’t built with these challenges in mind.
In this post, we’ll explore how neurodivergence and chronic illness can intersect, how one can exacerbate the other and practical strategies for managing these overlapping realities.
Understanding Neurodivergence and Chronic Illness
Neurodivergence refers to brain function that differs from what is typically expected. This includes conditions like:
- ADHD (Attention Deficit Hyperactivity Disorder)
- Autism Spectrum Disorder (ASD)
- Dyslexia
- Dyspraxia
- Tourette Syndrome and more.
People who are neurodivergent often process information differently, have unique strengths and face specific challenges in a world that caters to neurotypical ways of thinking and behaving.
Chronic illness, on the other hand, includes conditions like fibromyalgia, chronic fatigue syndrome (CFS/ME), asthma, lupus and many others. These conditions often cause persistent symptoms like pain, fatigue and cognitive issues, which can severely impact a person’s quality of life.
When neurodivergence and chronic illness coexist, they can intensify each other’s challenges. Here’s how:
The Impact of Cognitive Overload
One of the biggest challenges for neurodivergent individuals is managing cognitive load, or the amount of mental effort required to complete tasks. Conditions like ADHD or autism can make daily tasks more demanding, as they often require extra focus, planning, or energy to execute. Add a chronic illness to the mix and the cognitive load becomes even heavier.
Example: If you have ADHD, your brain may already struggle with executive functioning tasks like planning, organising, or remembering important details. When you also experience chronic fatigue or brain fog from a chronic illness, these tasks become exponentially harder. You may find yourself frequently forgetting medication doses, missing appointments, or feeling overwhelmed by daily responsibilities.
Practical Strategy: To manage cognitive overload, try using external tools like apps, reminders, or visual schedules to offload some of the mental burden. Apps like Todoist or Notion can help you keep track of tasks and appointments, reducing the stress of having to remember everything.
Sensory Sensitivities and Chronic Pain
Many neurodivergent people, especially those on the autism spectrum, experience heightened sensory sensitivities. This means that certain sounds, lights, textures, or smells can feel overwhelming or even painful. When you add chronic pain or discomfort from an illness like fibromyalgia, these sensitivities can become even more difficult to tolerate.
Example: Imagine you’re someone who is highly sensitive to touch and experiences chronic joint pain. Wearing clothing that feels restrictive or rough can become a source of distress, making it hard to get comfortable or focus on anything else.
Practical Strategy: Prioritise sensory-friendly clothing and environments. Invest in soft, loose clothing that doesn’t aggravate your pain and create a calming space in your home where you can retreat when things get overwhelming. Noise-cancelling headphones, weighted blankets and blackout curtains can also be helpful tools.
The Fatigue and Burnout Cycle
Fatigue is a common symptom of many chronic illnesses, but neurodivergent individuals may also experience fatigue from trying to mask their symptoms or fit into neurotypical expectations. For example, masking refers to the practice of hiding one’s neurodivergent traits to appear more “socially acceptable,” which can be mentally and emotionally exhausting.
Example: If you have autism, you might find social interactions draining and need extra time to recover afterwards. When you also have a chronic illness, that recovery time may not be enough, leading to a cycle of fatigue and burnout that feels impossible to break.
Practical Strategy: Give yourself permission to unmask and honour your body’s need for rest. Set boundaries around social interactions and high-energy activities and don’t be afraid to say no or cancel plans if you’re not feeling well. Self-compassion is key.
Emotional Regulation Challenges
Many neurodivergent people struggle with emotional regulation, meaning it’s harder to manage and recover from intense emotions. Chronic illness can exacerbate this, as pain and fatigue can make emotions feel even more difficult to control.
Example: You might experience heightened anxiety or irritability when you’re dealing with a flare-up of your chronic illness, making it harder to handle everyday stressors. Alternatively, the frustration of dealing with symptoms that limit your life can lead to feelings of hopelessness or anger.
Practical Strategy: Build an emotional regulation toolkit with strategies that work for you. This might include mindfulness practices, grounding techniques, or talking to a therapist who understands the intersection of neurodivergence and chronic illness. Apps like Headspace or Calm can offer guided breathing exercises and meditations.
Navigating Healthcare with Both Conditions
Healthcare systems are often not well-equipped to understand or support the overlap between neurodivergence and chronic illness. Many people face difficulties explaining their experiences to healthcare providers or advocating for appropriate care, especially if one condition is dismissed in favour of focusing on the other.
Example: If you have ADHD, you may struggle to remember or articulate your symptoms clearly during medical appointments. This can lead to feeling misunderstood or not taken seriously, particularly if your chronic illness symptoms are fluctuating or hard to measure.
Practical Strategy: Prepare for appointments in advance by writing down your symptoms, questions and concerns. Bringing a trusted friend or family member for support can also be helpful. Consider keeping a health diary to track your symptoms and share it with your healthcare provider for a clearer picture of your health.
Final Thoughts
Living with both neurodivergence and chronic illness can be incredibly challenging, but understanding how these conditions impact each other can help you develop more effective coping strategies. Remember, it’s okay to ask for help, use tools that make life easier and advocate for your needs, even when it feels tough.
If you think the overlap between neurodivergence and chronic illness might be affecting you, reach out to your GP or healthcare professional for advice. They can help guide you to the appropriate support and resources tailored to your unique situation.
For more tips and resources on managing life with chronic illness, sign up for my newsletter. You’ll receive weekly insights and practical advice to help you navigate your unique challenges. And don’t forget to follow me on Instagram @theemaspry for daily inspiration and community support.
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.

Read this post →
Living with and working alongside a diagnosis of fibromyalgia can feel like navigating an ever-changing landscape. With symptoms that often vary from day to day, it’s a condition that can make even the simplest tasks challenging. If you’ve been diagnosed with fibromyalgia, you know how frustrating it can be to cope with the unpredictability of your symptoms. But understanding your condition, recognising common triggers and developing practical coping strategies can empower you to manage your daily life with more confidence and ease.
In today’s post, we’ll dive into the key aspects of fibromyalgia: the symptoms you might experience, common triggers that can worsen your condition and strategies for managing the daily struggles that come with it.
Understanding Fibromyalgia
Fibromyalgia is a chronic condition characterised by widespread pain throughout the body, often accompanied by fatigue, sleep disturbances and cognitive difficulties (commonly referred to as “fibro fog”). The exact cause of fibromyalgia is still unknown, but researchers believe it may involve a combination of genetic, environmental and psychological factors.
The pain associated with fibromyalgia is thought to be related to how the brain processes pain signals. For many people, this condition can severely impact their quality of life, making it difficult to work, socialise, or engage in day-to-day activities. However, with the right strategies, it’s possible to find ways to manage your symptoms effectively.
Common Symptoms of Fibromyalgia
Fibromyalgia symptoms can vary widely from person to person, but here are some of the most common ones:
1. Widespread Pain: This is the hallmark symptom of fibromyalgia. The pain is often described as a constant, dull ache that affects multiple areas of the body.
2. Fatigue: Even after a full night’s sleep, people with fibromyalgia often feel tired and experience a lack of energy throughout the day.
3. Sleep Disturbances: Many people with fibromyalgia have trouble falling or staying asleep. Non-restorative sleep (waking up feeling unrefreshed) is also common.
4. Cognitive Issues: Often referred to as “fibro fog”, this symptom involves difficulty concentrating, memory lapses and a general sense of mental cloudiness.
5. Stiffness and Muscle Spasms: Some people experience morning stiffness or muscle spasms, which can make it hard to get moving.
6. Sensitivity to Touch, Light and Temperature: People with fibromyalgia may be more sensitive to touch, experience heightened pain from light pressure, or be unusually sensitive to temperature changes.
7. Headaches and Migraines: Frequent headaches or even migraines can be part of the fibromyalgia experience.
8. Digestive Issues: Many people with fibromyalgia also have gastrointestinal problems, such as irritable bowel syndrome (IBS).
Common Triggers for Fibromyalgia Flare-Ups
Fibromyalgia symptoms can come and go, but certain triggers can make them worse. Being aware of these triggers can help you take steps to manage flare-ups more effectively:
1. Stress: Emotional or physical stress can exacerbate symptoms. This includes work pressure, relationship conflicts, or even physical stress from overexertion.
2. Weather Changes: Many people with fibromyalgia report that their symptoms worsen in cold, damp weather or when there are significant temperature fluctuations.
3. Poor Sleep: Lack of restorative sleep can make pain and fatigue worse, creating a vicious cycle of poor rest and heightened symptoms.
4. Overexertion: Pushing your body too hard, whether through exercise or daily activities, can lead to increased pain and fatigue.
5. Diet: Certain foods, like sugar, processed foods, or dairy, may trigger symptoms for some people. Keeping track of how your body reacts to different foods can be helpful.
6. Inactivity: Interestingly, not moving enough can also worsen symptoms, as it may lead to increased stiffness and muscle pain.
Coping Strategies for Managing Fibromyalgia
While there’s no cure for fibromyalgia, there are ways to manage your symptoms and improve your quality of life. Here are some practical strategies:
1. Prioritise Rest and Sleep Hygiene
Since fatigue is a significant issue for many people with fibromyalgia, getting quality sleep is crucial. Establishing a consistent sleep routine and creating a restful environment can make a difference.
Tips for Better Sleep:
• Go to bed and wake up at the same time every day, even on weekends.
• Make your bedroom a calm, dark and comfortable space.
• Avoid screens and stimulating activities before bedtime.
• Consider calming bedtime rituals, like a warm bath or gentle stretching.
2. Practice Gentle Movement
Exercise can be tricky for people with fibromyalgia, but gentle movement is often recommended to help reduce stiffness and improve overall well-being. Low-impact activities like walking, swimming, or gentle yoga can be beneficial.
Practical Tip: Listen to your body and start with just a few minutes of movement each day. Gradually increase as your body allows and focus on exercises that don’t cause a pain flare-up.
3. Use Relaxation Techniques to Manage Stress
Chronic stress can exacerbate fibromyalgia symptoms, so finding ways to relax and reduce stress is essential. Techniques like meditation, deep breathing and progressive muscle relaxation can help calm your mind and body.
Practical Tip: Apps like Headspace or Calm can guide you through meditation and relaxation exercises, even if you only have a few minutes to spare.
4. Consider a Balanced Diet
While there’s no one-size-fits-all diet for fibromyalgia, many people find that eating a balanced, anti-inflammatory diet helps manage symptoms. Focus on whole foods, lean proteins, healthy fats and plenty of fruits and vegetables.
Practical Tip: Keep a food diary to track what you eat and note how it affects your symptoms. This can help you identify any foods that may be worsening your pain or fatigue.
5. Stay Warm During the Winter Months
As the cold weather can worsen fibromyalgia symptoms, make sure to keep warm and cosy during the winter. Use heated blankets, warm baths, or heat pads to soothe aching muscles.
Practical Tip: Dress in layers and use thermal clothing when going outside to protect your body from the cold. Having warm drinks throughout the day can also be comforting.
6. Seek Support and Connect with Others
Living with fibromyalgia can feel isolating, but you don’t have to go through it alone. Connecting with a supportive community, whether in person or online, can provide comfort, encouragement and practical tips.
Practical Tip: Consider joining a local or online support group to share experiences and learn from others who understand what you’re going through.
Final Thoughts
Managing fibromyalgia is a journey and it often takes time to figure out what works best for you. By understanding your symptoms, recognising your triggers and developing a toolkit of coping strategies, you can take steps to live a more balanced and fulfilling life. Remember, it’s all about listening to your body and making choices that support your well-being.
If you think fibromyalgia might be affecting you, reach out to your GP or healthcare professional for advice. They can help guide you to the appropriate support.
For more tips and resources on living well and working whilst managing a chronic illness, sign up for my newsletter. You’ll receive weekly insights and practical advice to help you thrive. And don’t forget to follow me on Instagram @theemaspry for daily inspiration and support.
Disclaimer:
The content in this blog is based on my personal experience of living with chronic illness and is shared for informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your GP or healthcare professional before making any changes to your lifestyle, work routine, or health management. The tips and strategies shared here can be used alongside medical advice to support your well-being.

Read this post →
I once believed that success meant pushing harder, sacrificing my health and soldiering on no matter the cost. Climbing the career ladder felt like the only way to prove my worth, but at my lowest point after my chronic illness diagnosis (crawling to the bathroom because walking was impossible) I knew something had to change. What I didn’t realise then was that chronic illness and neurodivergence weren’t the end of my story; they were the beginning of a transformation I could never have imagined. Here’s my story.
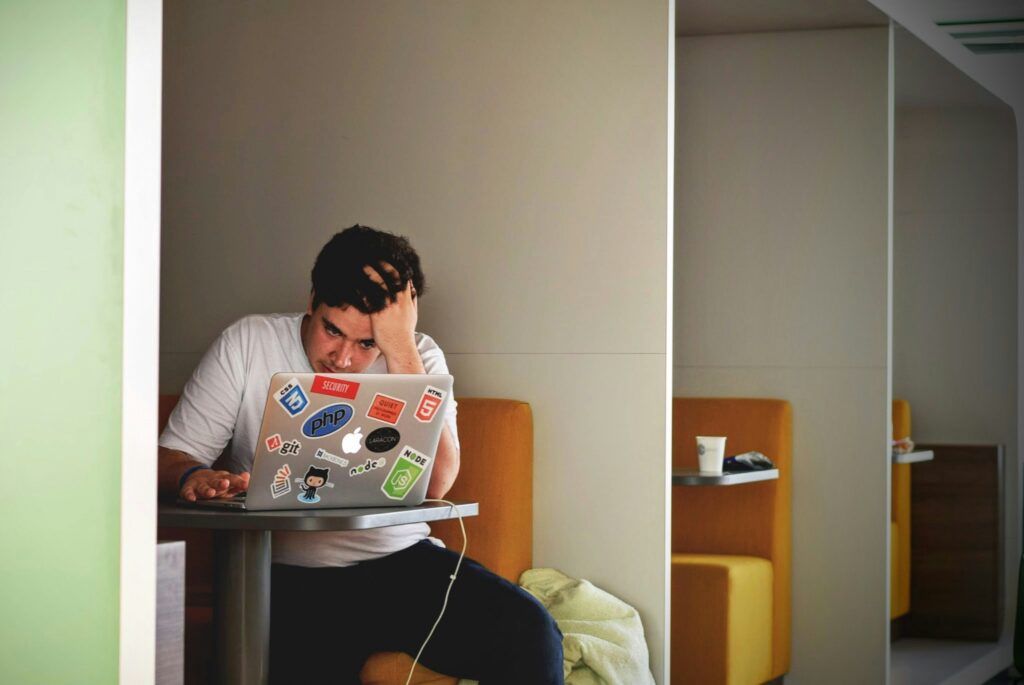
The Breaking Point
If you’ve ever felt like you’re running on empty, you’ll understand what I mean when I say my body gave up before I did. Exhaustion, brain fog and physical pain were constants in my life. I was grieving the loss of loved ones, juggling a demanding job and barely surviving. Outside of work, I had no energy for anything. My days blurred into a cycle of crawling to the bathroom, eating cold meals and sleeping whenever I could.
I thought I was just “bad at life.” But the truth was, I was in survival mode.
A Glimmer of Hope
Everything changed when I had to take sick leave. Staying with my mum gave me time and space to see that life didn’t have to look like this. A visit to a coastal housing development sparked something I hadn’t felt in a long time: hope.
Moving to a home by the sea didn’t magically fix my health, but it gave me the space to dream again. I started to reconnect with the person I was before chronic illness consumed my life. For the first time, I began to imagine a different kind of future.
Breaking Free
Years later, after maternity leave, I found myself back at a crossroads. The rigidity of a 9-5 job was suffocating and my symptoms returned. I took the leap into freelancing… A scary decision, but one that allowed me to create a career on my terms. Around the same time, I enrolled in a coaching programme, which helped me uncover the limiting beliefs I’d been carrying for years.
I realised I’d been measuring my worth by how much I could achieve, ignoring what I truly needed to thrive.
The Steps to Transformation
Rebuilding my life didn’t happen overnight, but every small, intentional step brought me closer to balance. Here’s what helped me:
- Rest and pacing: Learning to slow down and honour my body’s limits.
- Coaching and support: Challenging the beliefs that told me I wasn’t enough.
- Redefining success: Letting go of external validation and aligning my life with my core values.
With each step, I reclaimed my energy, my joy and my sense of purpose.
The Life I’ve Built Today
Today, I’m running a flexible business that aligns with my values of community, adventure and purpose. I have the energy to play with my feisty toddler, pursue my passions and dream big again.
Chronic illness is no longer an obstacle; it’s part of my unique story, helping me navigate life in ways I never thought possible. For the first time in years, I feel free.
A Message for You
If you’re reading this and feel like you’re stuck in survival mode, I want you to know it doesn’t have to be this way. Chronic illness doesn’t mean the end of your ambitions, it’s an opportunity to rewrite your story.
You deserve a life and career that works for you. One step, one decision, one mindset shift at a time, you can build the balance and fulfilment you’re searching for.
And you don’t have to do it alone.
If you’re ready to redefine success and create a career that aligns with your values, I’m here to help. My coaching sessions are designed to guide you through this transformation. Together, we’ll uncover what truly matters to you and build a life that honours your energy and ambition.
Let’s take that first step together. Book a discovery call to start your journey.

JOIN THE FAMILY
You may unsubscribe from these communications at any time. See our privacy policy for terms and conditions and to learn how we protect your data.
Become part of my family and get access to content that no-one else has!
Like practical tips, workbooks, resources and more, straight to your inbox 📧 Don't forget to tick the checkbox to receive these!